Cortisol Function: Ally or Foe?
Cortisol function is one of the most debated yet essential regulatory processes in the human body. Often labeled the “stress hormone,” cortisol plays a far more nuanced and complex role.
It helps us wake up in the morning, orchestrates metabolism, modulates immune responses, and enables our adaptation to change — whether it’s physical exertion or emotional upheaval. Cortisol can act as a protector that strengthens the body’s resilience or as a silent disruptor when its levels fall out of balance.
Recent studies increasingly link chronically elevated cortisol levels to the development of non-communicable chronic diseases — from hypertension and diabetes to depression and cognitive decline. That’s why understanding cortisol function and keeping it in check is becoming essential for those who aim to take control of their health beyond just symptom relief.
What Is the Function of Cortisol in the Human Body?
Among the most influential hormones in our body, cortisol plays a pivotal role. As a steroid hormone, its function is central to managing stress responses and maintaining internal balance.
When we face physiological or psychological challenges, cortisol springs into action, giving the body the ability to respond quickly to new demands. It increases the availability of energy by stimulating the breakdown of muscle tissue — which is why it’s considered a catabolic hormone. In cases of acute stress, when immediate action is needed, this mechanism proves highly effective. That’s why cortisol is often referred to as the “fight-or-flight hormone,” preparing the body to confront or escape perceived threats.
Let’s look at how cortisol function operates. The hypothalamus and pituitary gland regulate the release of cortisol from the adrenal glands. This hormone influences numerous vital systems — including cardiovascular function, metabolism, homeostasis, and the nervous system. Its role is equally important in maintaining cellular health and even supporting fetal development during pregnancy1.
Cortisol Function and Its Daily Rhythm
Rhythmicity is a defining trait of cortisol function. Its production follows a natural 24-hour cycle known as the circadian rhythm. In healthy individuals, cortisol levels peak approximately 30 minutes after waking. From there, they gradually decline throughout the day, reaching their lowest point at the onset of sleep.
IN THIS ARTICLE
3
5
RELATED ARTICLES
However, prolonged exposure to stressors can disrupt this delicate rhythm, leading to imbalances that may harm overall health. In its report “Mental health, resilience and inequalities” (Friedli, 2009), the World Health Organization (WHO) highlights how chronic, low-grade psychological stress activates neuroendocrine, cardiovascular, and immune systems. The report emphasizes the connection between prolonged cortisol production and the development of chronic conditions such as ischemic heart disease, stroke, diabetes, hypertension, metabolic disorders, and mental health disorders.
This underscores the critical role of cortisol function as a biomarker linked to a wide range of chronic diseases — and the need for early detection, screening, and targeted intervention strategies to address these risks effectively.\
Cortisol Function and Chronic Disease: Putting the Puzzle Together
Stroke
Stroke is one of the most severe and sudden threats to our health. Elevated cortisol levels, triggered by stress, have been identified as a significant factor associated with stroke risk. Elements such as high cholesterol, elevated triglycerides, blood sugar imbalances, and hypertension are often part of this picture — and stress may amplify them. Prolonged psychological stress can also increase blood clotting, making the blood more viscous and thus raising the risk of a stroke.
Recent studies have shed light on the link between cortisol function and stroke severity. High cortisol levels not only negatively affect the brain but also interfere with its ability to recover after a stroke.
Interestingly, low cortisol levels may also pose a risk. Research shows that individuals with insufficient cortisol production — often due to adrenal insufficiency — may experience higher mortality following a stroke. Up to one-third of stroke survivors suffer from post-stroke depression, and more than half report persistent anxiety even ten years after the event2. Yet, these findings open new perspectives for addressing the emotional and physiological aftermath of stroke.
» Tired and overwhelmed? Check your allostatic load — the science of stress impact.
Cardiovascular Disease
Research confirms that prolonged periods of stress and elevated cortisol levels have a profound impact on heart health. Chronic exposure to high cortisol can lead to increased levels of cholesterol, triglycerides, blood sugar, blood pressure, and visceral fat accumulation. Dekker et al. (2008) observed that elevated total cortisol is associated with a higher frequency of plaque buildup in the carotid arteries — a key indicator of atherosclerosis. A growing body of evidence also links cortisol with inflammatory processes that contribute to cardiovascular damage.
These findings highlight the critical importance of understanding cortisol function and the effects of chronic stress on the heart. Such insights may lead to more effective prevention and treatment strategies for cardiovascular disease.
Metabolic Disease / Type 2 Diabetes
Metabolic disorders, particularly type 2 diabetes, are now among the most widespread burdens of modern life. Unhealthy eating habits and sedentary lifestyles contribute to their rise — along with visceral obesity. Several studies also point to the significant role of stress3. Researchers have shown that chronic stress impairs regulation of the hypothalamic–pituitary–adrenal (HPA) axis, leading to insulin resistance4 and fat accumulation around internal organs. These changes can also trigger inflammatory responses that worsen metabolic health.
Inflammation and Autoimmune Disease
Prolonged elevation of cortisol alters both inflammatory and immune responses. High circulating cortisol interacts with immune cell receptors and promotes the release of pro-inflammatory cytokines5. This process contributes to systemic inflammation, immune suppression, and adverse metabolic outcomes.
Inflammation is also being closely studied in the context of cognitive disorders. The Alzheimer’s Association is exploring how chronic stress and cortisol exposure affect the immune system and the potential development of Alzheimer’s disease. While the mechanisms remain complex, active research is underway to better understand the link between cortisol function, long-term stress, and neurodegeneration, with the goal of identifying new therapeutic options.
Follow us on Facebook|| Instagram || Telegram || Youtube
📲 How to Use Cortisol Function Insights to Take Action
Your cortisol level on its own reveals little without the proper context. What truly matters is how it correlates with other biomarkers, how it reflects your adaptive capacity, and how vulnerable your body is to the long-term effects of stress.
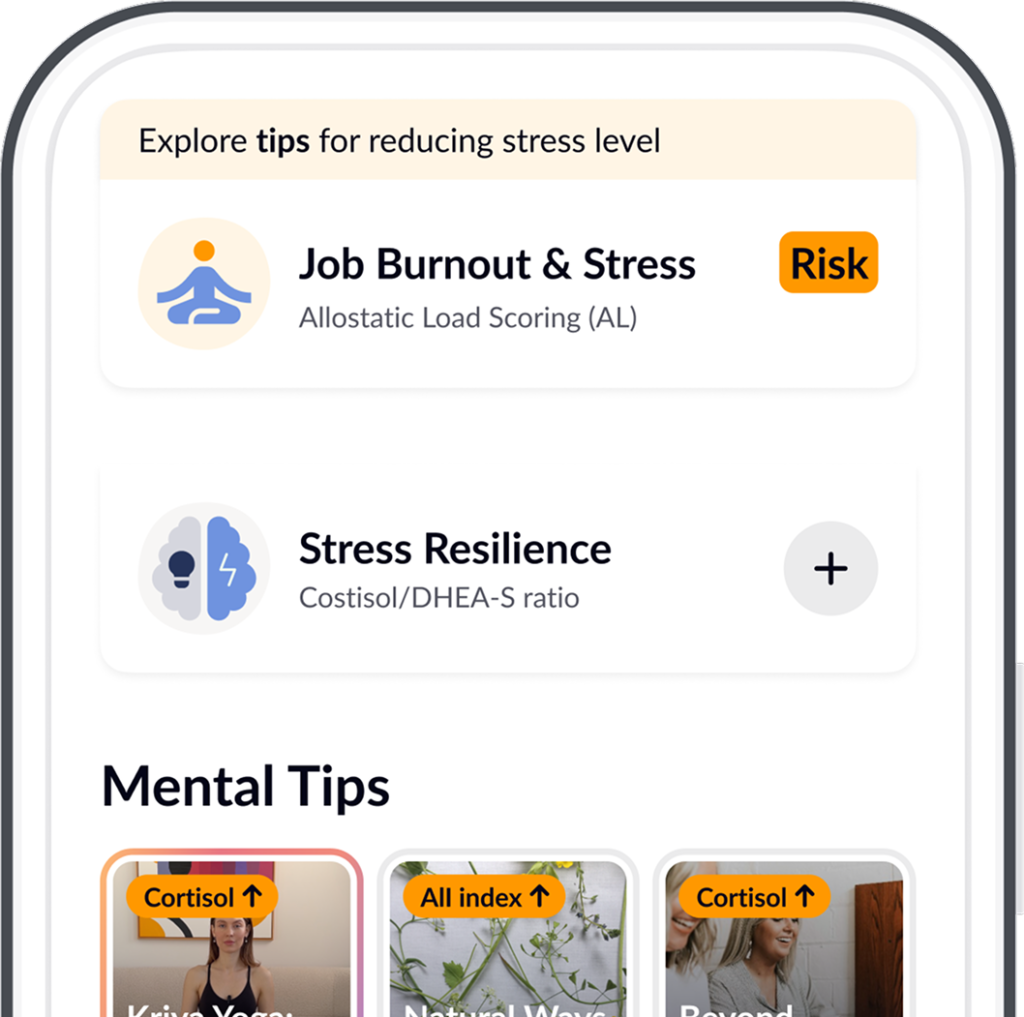
In the Healsens app, you can:
- calculate the cortisol/DHEA-S ratio to assess whether your body maintains a healthy balance between stress response and recovery,
- evaluate allostatic load — a measure of how chronic stress wears down your body over time,
- take a burnout screening test to understand how prolonged tension affects your mental and physical wellbeing.
These tools empower you to move beyond simply tracking cortisol levels. They help you uncover the hidden influences on your health, identify which habits, supplements, or practices are making a difference, and consciously take control of cortisol function in your daily life.
📲 Download Healsens and gain access to trusted tools for health assessment and personalized support.
Low and High Cortisol: When Cortisol Function Signals Deeper Health Issues
Low Cortisol
Both elevated and reduced cortisol levels can signal chronic dysfunction. Measuring cortisol in serum may assist in diagnosing adrenal insufficiency — a condition where the adrenal glands fail to produce enough hormones necessary for the body’s normal function. This deficiency can manifest in symptoms ranging from vague fatigue to life-threatening adrenal crisis. Often, diminished adrenal function remains hidden until the body is exposed to stress or illness.
Diagnosing adrenal insufficiency is complex, and a single test is rarely conclusive. When primary adrenal insufficiency is suspected, physicians typically evaluate serum cortisol, ACTH, renin, aldosterone, and perform additional biochemical testing.
In older adults, adrenal insufficiency is often secondary, meaning it is caused by another underlying condition that disrupts hormone production. Common lab findings in chronic primary adrenal insufficiency include anemia, hyponatremia (low blood sodium), and hyperkalemia (high potassium levels).
High Cortisol
Chronically elevated cortisol levels can disrupt multiple physiological systems. For instance, high cortisol slows digestion and promotes fat accumulation, particularly around the abdomen. It also affects physical performance:
- High cortisol can suppress testosterone production. Combined with cortisol’s muscle-degrading effect, this can impair muscle growth and recovery — a key concern for those training or recovering from injury.
- Elevated cortisol interferes with deep sleep. Normally, cortisol rises in the morning to help the body wake up. But persistently high cortisol can disturb circadian rhythms, impairing the ability to enter deep, restorative sleep — contributing to chronic fatigue.
- Cortisol suppresses the immune system — a topic we explore in more detail further on.
One of the most well-known conditions of chronic cortisol excess is hypercortisolism, also known as Cushing’s syndrome (CS). This condition presents with a wide range of symptoms, making diagnosis difficult and often delayed. First-line screening involves salivary cortisol testing, ideally collected in duplicate both in the early morning and late at night to evaluate the daily rhythm of cortisol function.
» Feeling lost in emotions? Discover the science behind the Mood Diary.
How to Check Your Cortisol Level?
The most informative way to assess your cortisol function is by measuring morning serum cortisol — ideally within 30 minutes after waking. This is when cortisol should naturally reach its peak, providing valuable insights into your body’s stress response and adrenal activity.
If you’re interested in understanding your stress resilience, it is advisable to check DHEA-S levels alongside cortisol. The cortisol/DHEA-S ratio offers a more complete picture of how well your body balances stress and recovery.
If you live in the Netherlands, Belgium, or Germany, you can easily get tested using the Healsens app.
Here’s how to order the test:
1. Download the Healsens app from the Google Play or the App Store, depending on your device.
2. Register in the app to unlock personalized features.
3. Go to “Browse Tests” and search for the Cortisol test.
4. Tap “Add to Cart” and complete your order.
5. Want deeper insight? You can optionally add the DHEA-S test to gain deeper insights into your adaptive capacity.
» This test is also included in the Vitality Check: 21 Biomarkers & Biological Age Kit — a popular starting point if you want a broader overview of your micronutrient status, energy, and biological aging.
Note
Not in the Netherlands, Belgium, or Germany, or using a different lab? No problem — you can have the recommended blood tests done at any local lab.
Then, manually enter your results in the Healsens app. Based on your data, you’ll receive:
✦ natural recommendations to help improve your values
✦ a complete health risk assessment
✦ personalized insights and follow-up guidance
Healsens remains your personal guide to preventive health — no matter where you are.
FURTHER READING
Source: ©️2019 Healsens B.V. All right reserved